Bariatric surgery is not about appearance. It is often about survival. Many patients turn to surgery after years of failed diets. Exercise plans may bring short wins, but results rarely last. The body resists drastic weight loss with powerful hormonal defenses. That resistance leads many to consider a surgical option.
A History of Failed Dieting and Rising Health Risks
Most candidates have tried every conventional method. They follow plans, lose weight, regain it—then repeat. Each cycle makes the body more efficient at storing fat. Obesity often escalates into diabetes, sleep apnea, or joint damage. Surgery enters the conversation when risks start to compound.
When the Scale Becomes a Symptom, Not Just a Number
Obesity is rarely just about food. It reflects metabolic conditions and emotional patterns. Weight becomes a sign of deeper imbalance. Doctors begin to see BMI not as vanity, but vulnerability. The higher the number, the greater the risks.
A BMI Over 40 or Over 35 With Comorbidities
Most guidelines start with a BMI of 40 or more. Or 35 if paired with conditions like hypertension or diabetes. This threshold shows the weight is affecting basic health. Surgeons won’t usually operate below those numbers. Unless extreme circumstances are clearly documented.
Obesity-Linked Illnesses Change the Urgency
A patient with obesity and uncontrolled diabetes faces a different path. Heart conditions raise the stakes further. Sleep apnea adds breathing difficulties and disrupts rest. These issues make surgery less optional and more urgent. Each case must be assessed in full context.
Emotional Readiness Is Part of the Equation
Surgery changes how people eat forever. The stomach is smaller, but hunger signals also shift. Patients must understand and commit to lifelong changes. Therapists often screen for emotional eating patterns. Mental health plays a larger role than many expect.
Weight Loss May Begin Before the First Incision
Doctors often require weight loss before surgery. This shows commitment and improves surgical safety. A reduced liver size helps the surgeon operate. Patients learn new habits before they’re required. That preparation is often key to long-term success.
Not Everyone Qualifies on the First Visit
Doctors do not schedule surgery at the first appointment. Evaluation includes blood tests, heart screening, and psychiatric review. Dietitians review eating patterns and calorie intake. The process often takes months before clearance is given. That delay filters out those not fully ready.
Age Is Considered, But Not a Final Decider
Teens and seniors both undergo bariatric procedures. For youth, maturity and support systems are key. Older adults must pass cardiovascular evaluations. There’s no strict upper or lower age limit. But suitability depends on resilience and goals.
Pregnancy Plans May Shift the Timeline
Women planning children must discuss timing with their team. Pregnancy within the first year post-surgery is discouraged. Nutritional needs change drastically during healing. Some patients freeze eggs or delay conception. Fertility often improves after weight loss.
Social Support Is a Predictor of Success
Surgery is one step—recovery is a lifelong climb. Family and friends help carry that load. Those with strong support tend to do better. Isolation can sabotage healing and long-term maintenance. Support groups fill critical gaps where needed.
Insurance Requirements May Shape the Path
Some plans require six months of supervised dieting. Others demand documentation from multiple specialists. Pre-authorization can take weeks or even longer. Paperwork often becomes part of the process. Without it, financial strain may block access.
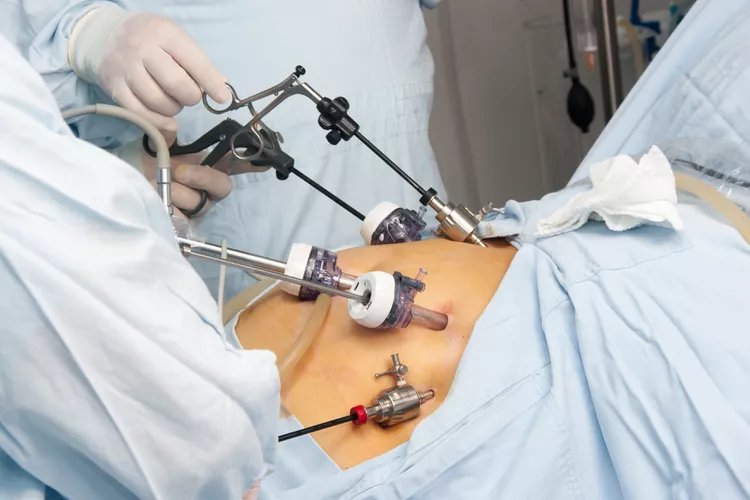
Choosing the Type of Surgery Isn’t Always Personal
Gastric bypass, sleeve gastrectomy, and banding each suit different profiles. Doctors recommend based on history and anatomy. Sleeve gastrectomy is now the most common choice. Bypass often helps with diabetes control. Patients rarely pick without medical guidance.
There Is No One Reason to Undergo Bariatric Surgery
Some want to walk without pain. Others fear early death. Motivations vary—but all are valid. What they share is this: current life has become unsustainable. Bariatric surgery offers a new structure to rebuild on. But it demands discipline, honesty, and long-term engagement.
Patients Must Own the Outcome Beyond the Operating Room
Surgery creates a new tool—but not a magic solution. Some regain weight if habits don’t change. Follow-up visits track nutrition, labs, and activity. Dumping syndrome discourages sugar and fat. Lifestyle choices determine the real outcome.
Long-Term Monitoring Is Not Optional
Patients stay connected with their care team for years. This includes dietitians, surgeons, and mental health staff. Deficiencies in B12, iron, or calcium are common. Screenings help catch issues early. Lifelong attention protects the gains made.
Source: Obesity Treatment in Dubai / Obesity Treatment in Abu Dhabi
